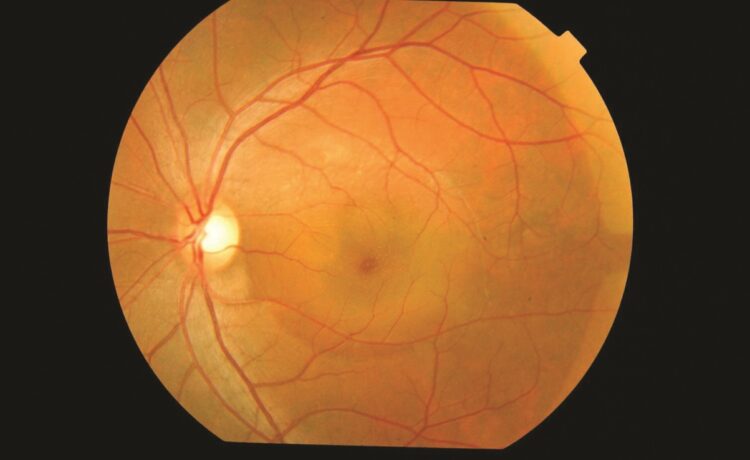
Central serous chorioretinopathy (CSCR) is an eye condition that results from fluid accumulation under the retina, leading to visual disturbances such as blurry or distorted vision. This condition typically affects young to middle-aged adults, especially men, and is often linked to stress, corticosteroid use, and other risk factors like hypertension and sleep disturbances. Early detection and diagnosis play a crucial role in effective central serous chorioretinopathy treatment, helping prevent long-term vision impairment.
What is Optical Coherence Tomography (OCT)?
Optical coherence tomography (OCT) is a non-invasive imaging technique that provides high-resolution cross-sectional images of the retina. By using light waves to capture detailed images of retinal layers, OCT allows ophthalmologists to assess structural changes in the retina, making it an essential tool in diagnosing various retinal diseases, including CSCR. The accuracy and depth of detail provided by OCT make it a preferred diagnostic method, as it helps differentiate CSCR from other retinal disorders.
How OCT Helps Diagnose Central Serous Chorioretinopathy
OCT plays a critical role in the diagnosis of CSCR by detecting subretinal fluid, assessing retinal thickness, and identifying abnormalities in the retinal pigment epithelium (RPE). When a patient presents with symptoms such as blurry vision, central vision distortion, or dark spots in their vision, OCT can confirm the presence of fluid buildup beneath the retina, which is characteristic of CSCR.
One of the most significant advantages of OCT in diagnosing CSCR is its ability to provide real-time, detailed images that allow ophthalmologists to determine the extent of fluid leakage and monitor disease progression. Additionally, enhanced-depth imaging (EDI) OCT helps visualize the choroidal layers, which can further aid in understanding the underlying mechanisms contributing to CSCR.
Differentiating CSC from Other Retinal Conditions
CSCR can sometimes be mistaken for other retinal conditions such as age-related macular degeneration (AMD) or diabetic macular edema (DME). OCT is instrumental in distinguishing CSCR from these conditions by identifying specific features unique to CSCR, such as:
- Localized subretinal fluid accumulation without significant leakage or widespread retinal damage.
- Thickened choroid, which is often a distinguishing feature of CSCR compared to AMD or DME.
- RPE irregularities, including pigment epithelial detachments that can be visualized using OCT.
By providing a clear and detailed view of retinal structures, OCT ensures an accurate diagnosis, reducing the risk of misdiagnosis and inappropriate treatment plans.
Monitoring Disease Progression and Treatment Response
Since CSCR can resolve spontaneously in some cases while requiring medical intervention in others, OCT is a valuable tool for monitoring disease progression and treatment response. Patients undergoing central serous chorioretinopathy treatment, such as laser photocoagulation, photodynamic therapy, or oral medications like mineralocorticoid receptor antagonists, require regular OCT scans to track fluid reduction and retinal health restoration.
OCT also assists in detecting recurrences, which are common in CSCR patients. Recurring episodes may necessitate a change in treatment approach, and OCT provides the necessary insights to guide ophthalmologists in making informed decisions.
The Limitations of OCT in CSCR Diagnosis
While OCT is highly effective in diagnosing and monitoring CSCR, it does have some limitations. For instance, OCT alone may not always reveal the exact cause of fluid leakage, necessitating complementary imaging techniques such as fluorescein angiography (FA) or indocyanine green angiography (ICGA). These additional tests provide further insights into choroidal circulation and pinpoint areas of active leakage that may not be apparent on OCT.
Another limitation is that OCT images can sometimes be affected by media opacities, such as cataracts or vitreous floaters, which may reduce image quality. In such cases, combining OCT with other imaging modalities ensures a comprehensive assessment.
Conclusion
Optical coherence tomography (OCT) has revolutionized the diagnosis and management of central serous chorioretinopathy by providing detailed, real-time imaging of the retina. Its ability to detect subretinal fluid, monitor disease progression, and differentiate CSCR from other retinal disorders makes it an indispensable tool for ophthalmologists.
While OCT has some limitations, when used alongside other imaging techniques, it offers a highly effective approach to diagnosing and managing CSCR. Accurate diagnosis with OCT ultimately enhances the effectiveness of central serous chorioretinopathy treatment, improving patient outcomes and preserving vision health.